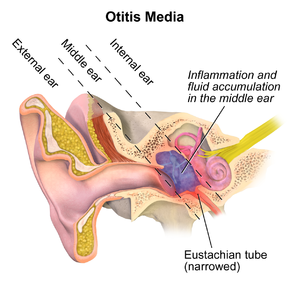
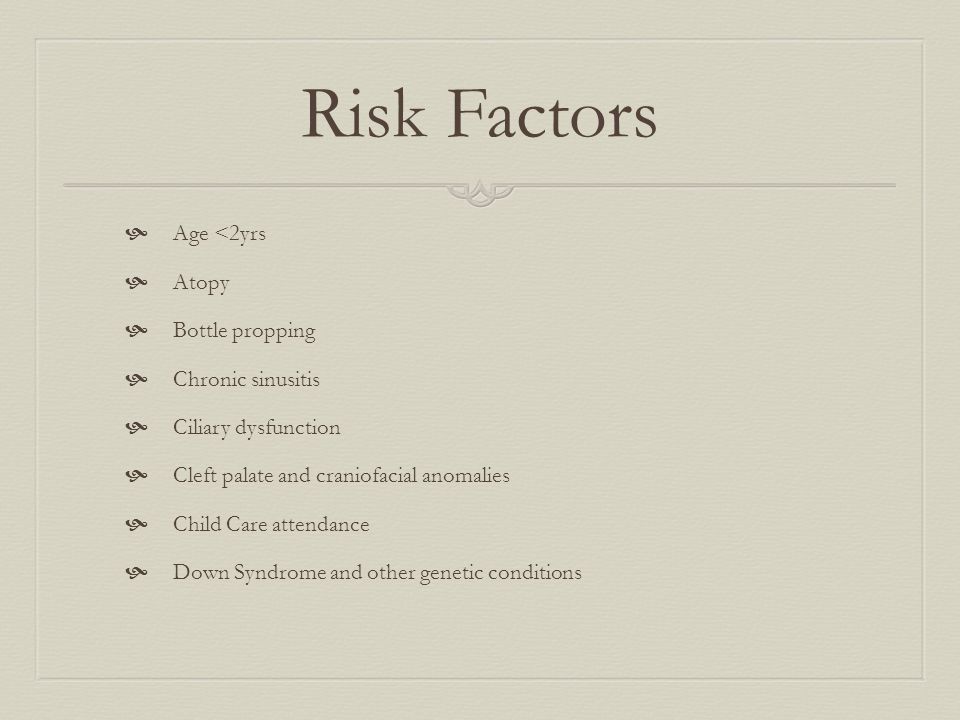
risk factors for otitis media
 Otitis Media: Diagnosis and Treatment - American Family Physician
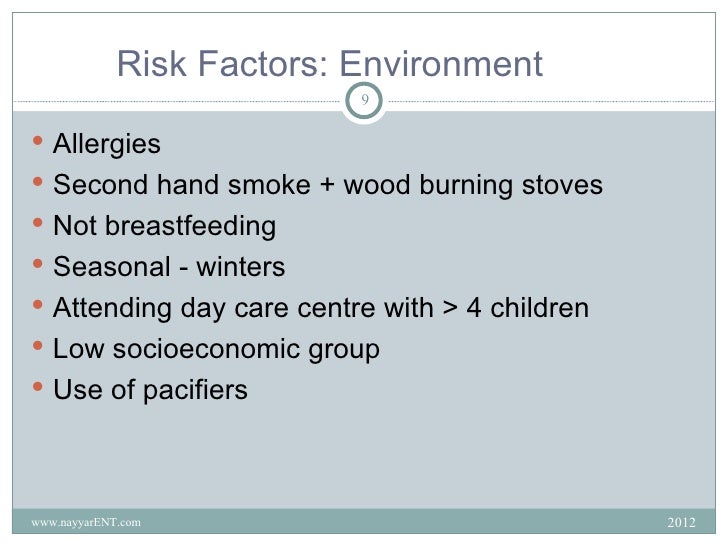
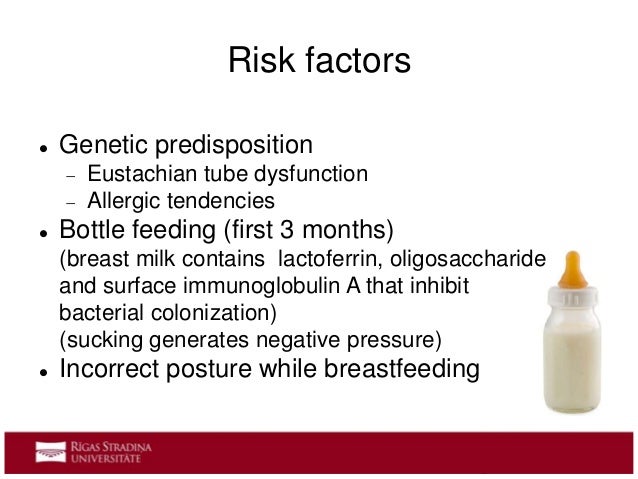
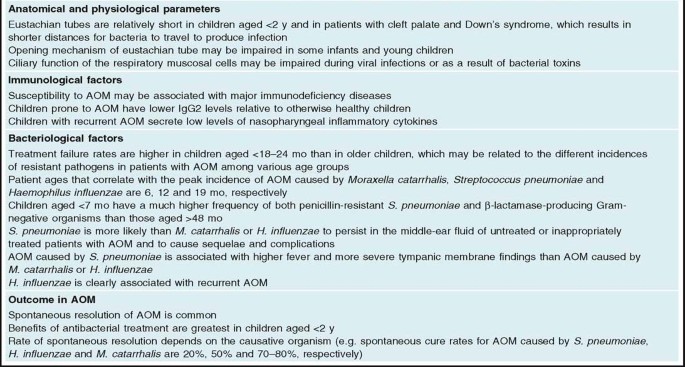
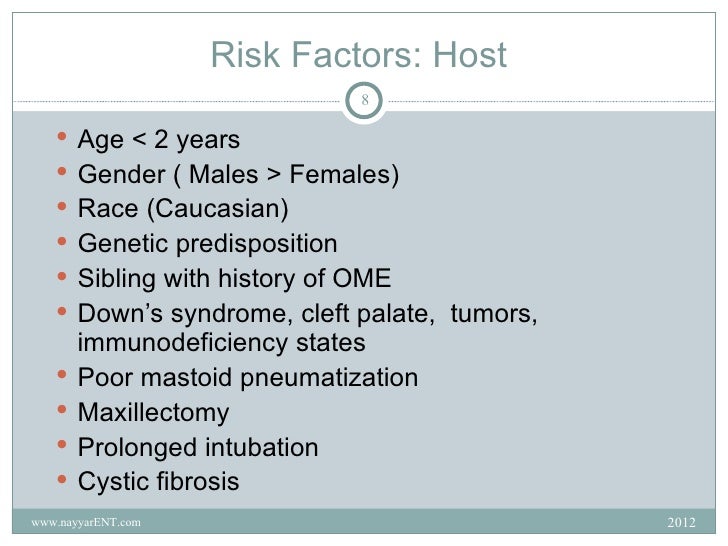
Otitis Media: Diagnosis and Treatment - American Family PhysicianWarning: The NCBI website requires JavaScript to operate. Risk Factors for Chronic and Recurrent Otitis Media-A Meta-Analisis Yan Zhang 1 Department of Otorhinolaryngology-HNS, Second Hospital, Faculty of Medicine, Xi'an Jiaotong University, Xi'an, China, Min Xu 1 Department of Otorhinolaryngology-HNS, Second Hospital, Faculty of Medicine, Xi'an Jiaotong University, Xi'an, China, Jin Zhang 1 Department of Otorhinolaryngology-HNS, Second Hospital, Faculty of Medicine, Xi'an Jiaotong University, Xi'an, China, Lingxia Zeng 1 Department of Otorhinolaryngology-HNS, Second Hospital, Faculty of Medicine, Xi'an Jiaotong University, Xi'an, China, Yanfei Wang 1 Department of Otorhinolaryngology-HNS, Second Hospital, Faculty of Medicine, Xi'an Jiaotong University, Xi'an, China, 2 Departments of Otolaryngology-HNS and Genetics, and Case Comprehensive Cancer Center, Case Western Reserve University, Cleveland, Ohio, United States of America, 3 Transformative Otology and Neuroscience Center, Binzhou Medical University, Yantai, Shandong, China, Qing Yin Zheng 1 Department of Otorhinolaryngology-HNS, Second Hospital, Faculty of Medicine, Xi'an Jiaotong University, Xi'an, China, 2 Departments of Otolaryngology-HNS and Genetics, and Case Comprehensive Cancer Center, Case Western Reserve University, Cleveland, Ohio, United States of America, 3 Transformative Otology and Neuroscience Center, Binzhou Medical University, Yantai, Shandong, China, Designed and designed the experiments: YZ MX. He performed the experiments: YZ JZ. He analyzed the data: YZ LXZ YFW. Reactive/material/analysis tools: YZ QYZ YFW. I broke the paper: YZ QYZ. Associated data(TIFF)(TIFF)(DOC)(DOC)Abstract Risk factors associated with chronic otitis media (COM) and recurrent otitis media (ROM) have been investigated in previous studies. The aim of this study was to integrate findings and determine the possible risk factors for COM/ROM based on our meta-analysis. A complete search of electronic bibliographic databases (Base PubMed, Embase, CNKI and Wanfang) was conducted from 1964 to December 2012, as well as a manual search for articles references. A total of 2971 articles were registered, and 198 full text articles were evaluated for eligibility; 24 studies were eligible for this meta-analysis. As for the risk factors for the COM/ROM, there were two or nine different studies of which the probabilities (OR) rates could be grouped. The presence of allergies or countertop increased the risk of COM/ROM (OR, 1.36; 95% CI, 1.13–1.64; P = .001). A higher respiratory tract infection (URTI) significantly increased the risk of COM/ROM (OR, 6.59; 95% CI, 3.13–13.89; PIntroductionThe media of chronic otitis (COM) and recurrent otitis (ROM) are two of the most common infectious diseases worldwide. COM and ROM affect various cultural and racial groups that are distributed in both developing and industrialized countries. A cross-sectional study conducted in nine countries on three continents revealed that the prevalence of diseases is significant enough to be considered for clinical practice. COM/ROM can cause hearing impairment and speech delay. COM can cause intracranial and extracranial complications. Effective treatment of diseases depends on a thorough understanding of risk factors. Risk factors significantly associated with the COM/ROM include ethnicity, genetic factors, gender, day-care centre assistance, breastfeeding and allergy/atopic, etc., as reported in previous studies. However, many of the studies reported were difficult to compare because they lacked clear case definitions, standard diagnostic criteria, or control groups to evaluate the possible prejudices of study. We perform a meta-analysis of all available published data and qualified studies that investigated possible risk factors for COM/ROM to clarify and propose possible means of treatment of the disease. Materials and Methods Research identification A literature search was done manually according to the search strategy () to evaluate risk factors for COM/ROM. We search for articles published in the Pubmed, Embase, WanFang () and China National Knowledge infrastructure (CNKI) (). Articles from 1964 to December 2012 were included in the search. The search was limited to humans and carried out without linguistic restrictions. The reference lists of the relevant original and revised articles were evaluated to identify additional studies. We use controlled vocabulary ( mapped out searches for MeSH terms or Emtree thesaurus terms) and text words for chronic otitis media, recurrent otitis media, middle ear cholesteatoma and mastoiditis. The concepts related to "Medium Otitis" were reviewed with the subheadings of congenital, epidemiology, genetics, immunology, microbiology and virology for all the terms of mesh in PubMed. Areas of focus that were chosen for otitis media in Embase were genetics, immunology and hematology, microbiology, otorhinolaryngology, pediatrics and public health. In addition, terms that indicated risks were also included, such as "risk factors", "probability", "risk experience", "risk situation", "causality", "emiological factors", "studiosepidemiological", "multitive analysis", " logistic models" and terms of entry. In general, 2547 Pubmed documents were recovered, 479 documents were recovered from Embase, 116 CNKI documents were recovered and 10 of Wanfang recovered. A total of 151 additional records were recovered from the manual reference search for related items. The workflow of this study follows the guidelines of the preferred notification articles for systematic revisions and metaanalysis (PRISMA) Declaration ().Comme/ROM DefinitionThe diagnostic criteria of COM/ROM were described in individual studies, which included case history, physical examination and other tests such as typogram, microscopic otocopia or typempanostomy tube inserts). The abbreviation COM includes the types of chronic suppurative otitis (CSOM) and the chronic media of otitis with effusion (COME). The means of chronic otitis with colesteatoma were not excluded from the definition COM, although no study related to that type was eligible for our metaanalysis. Table 1 Year of publication Risk factor Type of otits meida Type of study Age, years of participants Study durationNumber of cases Number of controls Total sample sizeStudy LocationEthnic GroupDiagnostic criteria of COM/ROMStahlberg, M. R. 1986 Assistance to the day care center, passive smoke, under socioeconomic statusROMCase-control10–44 months in case group, 14–38 months in control groupMarzo, 1983–Feb, 1984115222337 Turku, FinlandRooms in Turku, Finland Three or more episodes of OMEDaly, K. 1988Sex, Assistance to Day Care Centers, White People, Allergy, Family History of the WTOOMECase-control10 months - 8 yearsJan, 1982-Sep, 1984177182359 Minnesota, USA White Villages and Other Unidentified Populations The MEE persisted in one or both ears in visits of 3 and 6 weeks, or AOM without MEE resolution during the 6 weeks Fliss, D. M. 1991 History of AOM/ROM, Assistance to the day care center, Larger and more brothers, Sex, Allergy, Sinusitis and recurring URTI, Maternal Feed, Passive FumeCSOM without Cholesteotoma Case-control2–15 yearsJan, 1987-April, 19908876164Southern Israel Jewish population Continuous otorrine ≥2 months Kalm, O. 1994HLA FrequentCSWHOE Average age 16.4Follow-up 11.1 years401701 for HLA-A and B 438 for HLA-C 102 for HLA-DR1741 SwedenNo commentThe secretion of chronic or recurring mid-heard persists for at least 6 years. Kvaerner, K. J. 1996 Birth weight, gestational ageROMCase-controlBefore age 7Baby born between 1967–197451953455864Norway Norwegian twin pairsNorthletes Current ear infections Ilicali, O.C. 1999 Passive smoke, SexROMNext3-7 yearsMay 1st, 1995– November 30, 1996166166332Istanbul, TurkeyPatients of the Istanbul School of MedicineExtensive bilateral OM for at least 3 months or 6 months unilateral. ≥3 episodes of AOM for 6 months prior to or at least 4 episodes during the previous year. Juntti, H. 1999 Alergia de la leche de vacaROMCase control9-11 years old. Average age = 10.5±0.6 years1986-198756204260Finland Local residents15 episodes of OM in 10 years Engel, J. 2001 Sex, gestational age, Birth weightCOMECohorte prospectiva2 years old2 years of follow-up434083 NetherlandNewborns from Maastricht University HospitalOtoscopy and typempanoetry exam to evaluate combined with MOMES diagnosis-algorithm Ilicali, O.C. 2001 Fuma passiveROMNext3-8 yearsOct, 1996-Apr, 199811440154Istanbul, TurkeyLocal residentsOME persisted for ≥3 bilateral months or 6 unilateral months. ≥3 episodes of RAOM for 6 months prior to or ≥4 episodes during the previous year. Ramet, M. 2001 Manufacturing proteins- FrequenciesROMCase-control1–10 years old, mean age = 8.4±5.2No comment147228375 FinlandLocal and resident Patients At least 5 episodes of AOMDaly, K. A. 2004 Support for the link to chromosomes 10q and 19q, assistance to the day care center, Exclusively fed with formula, passive fumaCOME/ROMRetrospective cohort Family members, age not mentioned 1992–2001371245616Minnesota,USA Families excluded from the University of Minnesota Sympanostomy Tube Surgery for COME/ROMKeles, BUSA 2004 Pharyngeal refluxCOMECohorte prospectiva3-7 years, mean age = 6±3.1No comment251237 Konya, Turkey No commentCOME √3 months Engel, J. A. 2005 Maternal food, day care center assistance, family history of OM, passive smoke, URTI, mother smoking during pregnancy, use of medicines during pregnancyROMCohorte prospective2.1-7.5 yearsDec, 1999-Ago, 2003731790 Nijmegen and Winterswijk, Netherlands No comments MEE at least 3 months Chantry, C. J. 2006 Breastfeeding ROMCohorte prospective6–72 months old 1988–199488271359USA Black, Mexican 3 episodes of OMGozal, D. 2008 Snoring, African American, Chronic nasal obstruction, Allergy, Ahumado passiveROMRetrospective choke5–7 years1999–200450741124716321Louisville, USAAfrican American and other unclassified ethnic groups History of ROM and insertion of tubes typempanostomyLasisi, A. O. 2009 Serum retinol levelCSOMSiguiente6 months–7 years, mean age = 7.8 years No comment11652168Ibadan, Nigeria No CommentsOtorhoea resistance ≥3 months Lasisi, A. O. 2007URTI, Inner cuisine, Allergy, low social group, passive smoke, maternal food, attendance at day care centerCOMECase-Control30 days-14 years No comment189100289 Nigeria No Comments≥3 episodes of OM in 1 year Schejbel, L 2009 Deficiency ProperdinROMRetrospective cohort All age of three generations of a familyNo comment42125 Denmark IndioSeveral episodes of OMBakhshaee, M. 2011AlergyCSOM prospective cohort10–50 years, mean age = 30 years) No comment68184252 Mashad, IranNo commentCSOM diagnosed at least 1 yearElemraid, M. A. 2011 Additional factorsCSOMCase control study0.6–15 years (medium = 6.0) in case group 0.9–15 years (medium = 8.2 in control groupMarch to May 20077574149 Sana'a Yemen, CSOM diagnosis and history of persistent ears of discharge for at least 2 weeksJensen, R. G. 2011Sex, Ethnicity, Mother's Low Education, Family History of COM, Mother's FoodSECOMNext11–15 years1996–200845191236Nuuk and Sisimiut, GreenlandInuit, Danish, Mixed ≥2 weeks of orrhea for ≥3 monthsNelson, H. M. 2011 Overweight in young children ROMCohorte prospective1 month-27 months. Average age = 24.1 months1991–1996203227430 Minneapolis, USA ROM treated with tubes of typempanostomy Sale, M. M. 2011 Assistance to the day care center, breast food, AllergyCOME/ROMCase-ControlMean age = 5.9 in case group. 5.4 in control groupOct, 1996 - Abr, 1998380238618Istanbul, TurkeyLocal residentsOME or ROM treated with ventilation tubesStudy Selection and QualityWe included the study of prospective cohort, case cohort and annihilated design of case control, case control or case anacing, retrospective case control and cross-sectional studies. The included publications should meet the following criteria: Inclusion of human subjects Clear definitions of COM/ROM and estimation of the association of relative risks (dangers detection, risk factors) of COM/ROM; Numbers for both controls and COM/ROM cases; Sufficient data are to determine the probability ratio (OR) with confidence intervals of 95% (CIs). We exhibit descriptive studies, case reports, case series, revisions, letters, comments and studies on pathogenesis and the treatment of COM/ROM. Repeated reports were excluded with a small number of participants and these data were included in major studies mentioned above. We excluded studies of recurrent acute otitis media, congenital cholesteatoma and unclassified OM. The inclusion discrepancy was resolved in joint discussions of the researchers. We appreciate the quality of the studies, focusing on the selection of cohorts and the evaluation of the results. Data extraction Two researchers (Yan Zhang and Jin Zhang) independently extracted and recorded the data from the eligible publications. The following data were extracted from each article: author, year of publication, risk factor, type of average otitis, type of study, age/year of participants, duration of study, number of cases, number of controls, total sample size, location of study, ethnic group and diagnostic criteria for COM/ROM. All disagreements were resolved through group discussion. Statistical Analysis The meta-analysis was processed using the Revision Administrator 5.1, version: 5.1.6. It is estimated that the probability rates (OR) and confidence intervals of 95% (CI), and the statistical heterogeneity of the studies was evaluated before combining the results. The estimates of risk factors were maintained using a random effect model. The inconsistency of studies was quantified by the use of I2 statistics, which describes heterogeneity among studies. The I2 values of 50% reflect the low and high heterogeneity, respectively. A sensitivity analysis was performed by calculating the results after a single study was omitted in each shift. Finally, the publication bias was evaluated using funnels (see ). ResultsLiterature Search and selection of study Of the 2971 identified relevant references, 198 articles were considered potentially relevant. Excluded references considered irrelevant included examinations, letters, comments, studies on pathogenesis, pathologies and treatment, and microbiological studies. A total of 103 case control or cohort studies examined the risk factors of COM/ROM, and 79 studies did not meet the inclusion criteria for the following reasons: unclear definition of COM/ROM, non-grading of OM, non-control groups and insufficient data for abstraction. For repeated studies, we retain one with the largest sample size. Figure 1 shows the selection flow for this metaanalysis; 24 independent studies met all the inclusion criteria, –. The characteristics of the studies included are summarized in .Analysis of risk factors The data obtained from 7 studies indicated the presence of allergy or atopedia and increased the risk of COM/ROM (OR, 1.36; 95% CI, 1.13–1.64; P = .001). A total of four studies investigated the association between the upper respiratory tract infection (URTI) and COM/ROM, which includes the presence of cough or rhinorrhea or nasal filling or throat pain or denoid or denoid adenoiditis/hitrophy. The data grouped showed that URTI significantly increased the risk of COM/ROM (OR, 6.59; 95% CI, 3.13–13.89; Factors that were determined not to be significantly associated with higher risk included chronic nasal obstruction (OR, 1.19; 95% CI, 0.84–1.69; P = .34), male (OR, 1:24; 95% CI, 0.95; The data grouped revealed that an association between breastfeeding √6 months and the COM/ROM was not statistically significant (OR, 0.57; 95% CI, 0.17–1.93; P = .36), nor was it an association between breast feeding (yes/no) and COM/ROM (OR, 0.91; 95% CI, 0.47–1.79; P = .79). The risk factors grouped for COM/ROM are summarized in and .Table 2Risk factor Number of studies[references]No of subjectsOR95% CIP valueI2 (%)Alergia/Atopy7 , , , , , , , 182631.36[1.13, 1.64]0.00126 Upper respiratory tract infections4 , , , 8656.59[3.13, 13.89] Chronic nasal obstruction2 , 166101.19[0.84, 1.69]0.3454Snoring2 , 164111.96[1.78, 2.16] 14351.24[0.99, 1.54]0.060 Assistance to day care centers7 , , , , , 24541.70[0.95, 3.05]0.0789 Family history of media otitis4 , , 11661.40[0.86, 2.28]0.1852 AOM/ROM2 patient history, 42511.13[1.06,116.44]0.0494Passive Humo9, -, , , 188761.39[1.02, 1.89]0.0480 Low social status group2 , 6003.82[1.11, 13.15]0.0382 Low-Mother Education Level2 , 4951.68[0.32, 8.68]0.5490 Mother smokes during pregnancy2 , 4222.34[0.64, 8.54]0.2070 Larger and more sibling families2 , 4251.57[0.93, 2.63]0.095 Breastfeed 6 months2 , 9120.57[0.17, 1,93]0.3688 Breastfeeding (yes/no)3 , , 13630.91[0.47, 1.79]0.7986 Other research on risk factors for COM/ROMs included in our eligible studies included HLA frequencies, nutritional factors, use of medicines during pregnancy, Greenlandic ethnic groups, White, African American, duedin deficiency, covered cuisine, pharynge reflux, overweight state, older brothers, dietary history, serum retinol, genome for loci of 10qine, Prote Unfortunately, only one research group reported each previous risk factor, which made the data unavailable. There was an association between the gestational age and the COM/ROM of two research groups, but the birth weight and the COM/ROM of these groups applied different criteria and made it impossible to combine data. DiscussionCOM/ROM is a disease with different etiologies possible. Using a meta-analysis design using strict diagnostic and inclusion criteria, we conduct a reliable study to investigate the risk factors associated with the disease. This study is the best of our knowledge the first metaanalysis that investigates risk factors for COM/ROM. There are two published studies on risk factors and the etiology of AOM , . Allergy or atopia is a significant risk factor for COM/ROM. Inner allergens and respiratory allergies such as allergic rhinitis contribute to the beginning of COM/ROM. The prevalence of atopic conditions, including allergic rhinitis in COM/ROM patients, ranges from 24 to 89%. New evidence of cell biology and immunology explained allergy as a cause of blockage of the euskera tube (ET). People with allergic or atopic conditions are more likely to suffer from COM/ROM. The upper respiratory tract (URTI) infection, which includes coughing or rhinorrhea or sore throat, was indicated as a significant prognostic factor for COM/ROM. Studies support that the mucous condition of ET could be affected by URTI. A previous or concurrent viral URTI, as well as a polymicrobial disease, is considered one of the risk factors for the start of OM. Viral URTI promotes the replication of bacterial infection and increases inflammation in nasofaringe and ET.The ronchi, defined as the presence of strong snoring at least three times a week, is a common symptom in children and is very common in children. Eligible studies in this meta-analysis suggested that the risk of COM/ROM seemed to be related to the presence of snoring. The snoring is determined physiophysiologically by the size of the lymphoid tissue of the upper airway. The underlying mechanism of snoring and COM/ROM appears to be increasing the resistance to the upper airways, as well as the dysfunction of the euskera tube. Early assessment and intervention in children with strong snoring can prevent them from developing middle ear diseases. The previous history of AOM/ROM was studied as a predictive factor for COM/ROM. Subjects who experience episodes of AOM/ROM have a higher risk of developing chronic and recurrent infections in the middle ear. Second-hand smoke has been reported to be associated with increased prevalence of middle ear diseases. In meta-analysis of risk factors for acute otitis media, it was concluded that parental smoking increased the beginning of acute middle ear infectious disease in children. In our study, the same conclusion was reached on second-hand smoking as a significant causative factor contributing to the morbidity of the COM/ROM. Several studies suggest that nicotine and other smoking products could make subjects more susceptible to ear infections and improve the possibility of the invasion of the microorganism in the middle ear. Exposure to smoke could damage the mucociliar function of the ET, resulting in the blockade of the nasofaring airway. The adherence to the microorganism to the epithelial cell surface and the depression of the local immune function were investigated as the pathogenetic mechanism of the occurrence of the middle ear disease caused by the Second Hand tabaquism. Effective methods should be adopted urgently to reduce the prevalence of smoke exposure. The possibility that the COM/ROM is associated with low social status has been debated for a long period of time. Our data from two eligible studies considered the social prestige of professions and occupations, as well as the income of parents. Statistical data revealed that patients with COM/ROM were more often belonging to low socio-economic conditions than controls. Several reports on this danger originated in poor housing, environmental and occupational conditions, and the difference between the risk of average otitis in various studies has been estimated. Apart from a conclusion that male sex was more likely to suffer from acute otitis media in children, our study found no meaning in the difference between male and female morbidity of COM/ROM. Breastfeeding is believed to provide antimicrobial, anti-inflammatory and immunomodulatory agents that contribute to an optimal immune system. The relative contribution of breastfeeding to the prevention of middle ear infections has been reported in many studies. It is reported that breast-feeding, even for only 3 months, could decrease the risk for acute otitis media in children . However, patients with COM/ROM do not differ from the control group in this regard in our study. The study on the preventive effects of breastfeeding for 6 months found no statistical importance within the control group. Even without breastfeeding, the impact on the incidence of COM/ROM seemed to be unnamed in our meta-analysis. Assistance to the daily care centre could increase the risk of exposure of children to respiratory pathogens. It has been reported that it is a significant risk factor for acute infectious respiratory diseases in children, , . However, this was not consistent with some other studies. In this meta-analysis, there was no association between COM/ROM and assistance to the day-care centre. The causal relationship among other factors, including chronic nasal obstruction, the family history of otitis media, the mother's smoking during pregnancy and the COM/ROM is not fully established. The association between larger families and more brothers with COM/ROM was not statistically significant. Genetic predisposition is considered an important prognostic factor that could influence the risk of otitis media. Previous genetic studies associated with a number of immune system genes with average otitis, including TNF-α, IL-6, IL-10, Tlr4, surfactant, CD14, FcRIγIa, IFNγ, Eya4, p73, MyD88, Fas, E2f4, Plg, Fbxo11 and Evi1 . Other genetic predispositions include HLA frequencies and properdin deficiency. Unfortunately, eligible studies included in our metaanalysis investigated defects of individual genes in each study, which made it impossible to collect data and make a conclusion. Similar to risk factors for genetic predisposition, other risk factors for COM/ROM prevented data from being kept in our eligible studies; these include nutritional factors, use of medicines during pregnancy, Greenland, White, African American, indoor cooking, pharyngeal reflux and overweight status. The association between the gestational age and the COM/ROM of the two groups, , birth weight and COM/ROM of the same groups applied different criteria and therefore made it impossible to combine the data. We realized that sex risk factors, attending day-care centers, large families and more brothers have p values of 0.06, 0.07 and 0.09 respectively. With the application of the value of 0.05 p, which is the criterion of conventional use, no importance was found. Using a 10% cut to mean can improve this problem but could increase the risk of drawing a false positive conclusion (type I error), . However, these three risk factors should be considered at least as a strong risk factor trend for COM/ROM. When judging the inconsistency of studies, I2 was applied to test heterogeneity. In our non-incoherence studies (I2 = 0) or low heterogeneity (I2A complete understanding of the etiological factors for COM/ROM could be beneficial for the treatment and prevention of the disease. Our study evaluates risk factors through an objective scientific procedure, metaanalysis, to provide evidence of precise causal prophylaxis. Metaanalysis is widely used in randomized clinical trials medical studies as well as etiological factors of the disease. The polemic of meta-analysis is in the homogeneity of studies. Dickersin and others noted that heterogeneity is not so bad, . Improves the generalization of metaanalysis results. The common estimates of probabilities ratios are valuable and important indicators to assess the risk factors of a disease. The heterogeneity of risk factors is carefully calculated and the results are interpreted with caution in our study. Conclusions Risk factors for COM/ROM are closely related. Our meta-analysis identified reliable conclusions that allergy/atopia, upper respiratory tract infection, snoring, previous history of AOM/ROM, second-hand smoke, low-social status are important risk factors for COM/ROM. Other unidentified risk factors researched in individual studies need possible repeated studies with critical criteria to be properly estimated. We suggest that the previous risk factors of COM/ROM be effectively interfering to prevent and decrease the onset of the disease. Support information Figure S1 Funnel. Simetric reverse funnel form indicates improbable publication bias.(TIFF)Figure S2 Risk factors for COM/ROM. Eligible studies probabilities coverage analyzed in the risk factor metaanalysis for COM/ROM(TIFF)Checklist S1 PRISMA checklist. (DOC)Text S1 Search strategy. (DOC)Recognition We thank Qian Wu for statistical analysis and Sherrie Irwin for language editing. Funding status This work was supported by the National Natural Science Foundation of China [30973300 to M.X.] and the Key Clinical Programme of the Second Hospital, Xi'an Jiaotong University [YJ(ZDJH)201103 to M.X.]. Funders had no role in the design of study, data collection and analysis, the decision to publish or the preparation of the manuscript. ReferencesFormats: Share , 8600 Rockville Pike, Bethesda MD, 20894 USA

Predisposing factors of Otitis Media with Effusion (OME) | Download Table

PDF) Predisposing factors for acute otitis media in infancy

Pediatric otitis media: To treat or not to treat with antibiotics - American Nurse
Management of Pediatric Otitis Media

Risk factors of acute otitis externa seen in patients in a Nigerian tertiary institution Abdullahi M, Aliyu D - Sahel Med J

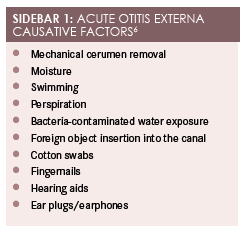
Acute Otitis Externa: An Update - American Family Physician

References in Otitis media - The Lancet

Knowledge of caregivers on the risk factors of otitis media Adeyemo AA - Indian J Otol
Otitis media with effusion ome

Management of otitis externa and the veterinary nurse's role | The Veterinary Nurse

Acute Otitis Media and Otitis Media with Effusion | Ento Key
Acute otitis media

Table 1 from Acute Otitis Media- An Update | Semantic Scholar
PLOS ONE: Risk Factors of Early Otitis Media in the Danish National Birth Cohort

Chronic Otitis: A Dermatologist's Perspective on Surgery | Today's Veterinary Practice

Management of Otitis Media with Effusion (OME) in primary care - ppt video online download

Otitis Media in Young Children - Mayo Clinic Proceedings

Acute Otitis Externa: An Update - American Family Physician

Translating Recent Microbiome Insights in Otitis Media into Probiotic Strategies | Clinical Microbiology Reviews

Acute Otitis Media in the 1990s: The Impact of Antibiotic Resistance

Table 1 from Otitis media with effusion and atopy: is there a causal relationship? | Semantic Scholar

Risk Factors of Otitis Media with Effusion in Children

Lightning Learning: Otitis Media (Diagnosis & Management) — #EM3: East Midlands Emergency Medicine Educational Media
The use of antibacterials in paediatric patients with acute otitis media depends on patient age and disease severity | SpringerLink
Pathology of Otitis Media - Dr Sampurna Roy MD
Otitis media - Wikipedia
Effective Treatment for Acute Otitis Externa | Contemporary Clinic

Knowledge of caregivers on the risk factors of otitis media Adeyemo AA - Indian J Otol
Otitis Externa: Investigation and Evidence-Based Treatment (29.03.2019)
Otitis media with effusion ome

Acute otitis media in adults - UpToDate
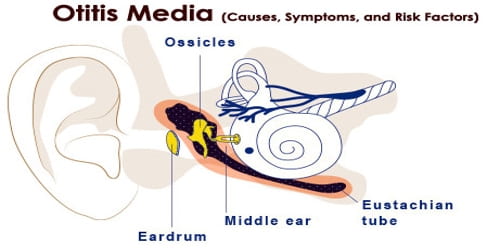
Otitis Media (Causes, Symptoms, and Risk Factors) - Assignment Point
AOM. Otitis Media Otitis Media with effusion (OME) Acute Otitis Media (AOM) Recurrent AOM Chronic Otitis Media/Chronic Otitis Media with effusion. - ppt download

Chronic Suppurative Otitis Media - Clinical Evidence Handbook - American Family Physician

Otitis media with effusion and atopy: is there a causal relationship? - ScienceDirect

Fillable Online RISK FACTORS FOR OTITIS MEDIA WITH EFFUSION IN Fax Email Print - PDFfiller

Prescribing for upper respiratory tract infection | Practice Nursing

Risk Factors Responsible for Acute Otitis Media in Infancy and Children Less than Five Years: A Case-control Study | Clinical Medicine | Epidemiology

Otitis media in children Picardo N, John M - Curr Med Issues
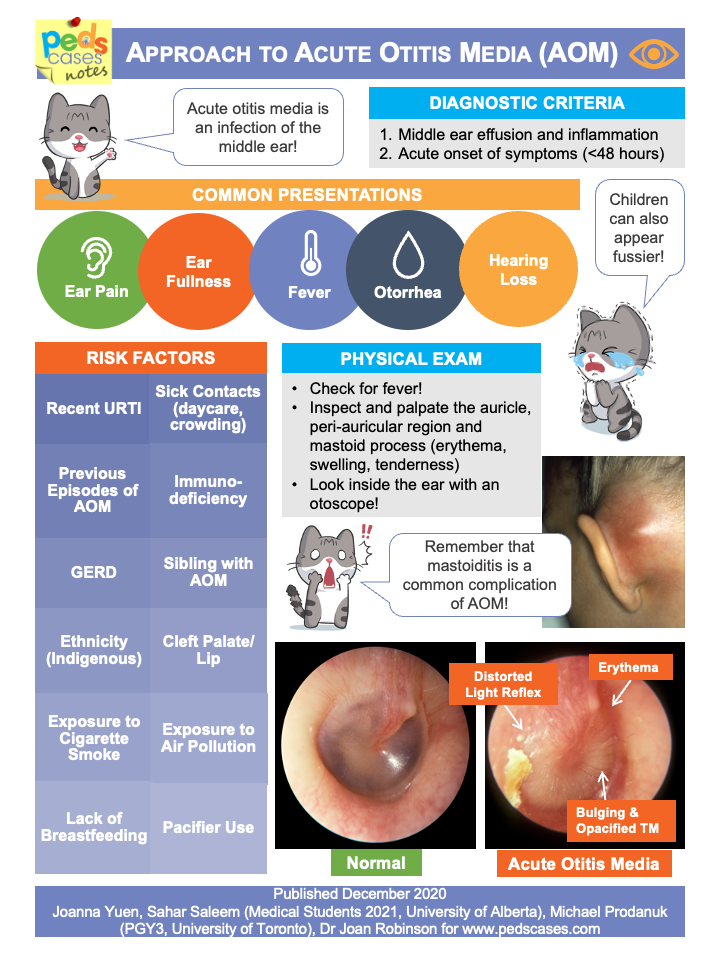
Acute Otitis Media | PedsCases
Posting Komentar untuk "risk factors for otitis media"